Vitamin C Dosage For Histamine Intolerance
At the beginning of my healing journey with Hashimoto's, I experienced many allergies and sensitivities. It truly felt like I was allergic to everything, including all of the trees and bushes in California, as well as my sweet dog!
Many readers in this community also report symptoms of histamine intolerance, which can be challenging to differentiate from other food sensitivities and imbalances in the digestive system. The good news is that many seemingly different symptoms will have the same root causes. When we get to the root, whole body healing can happen.
Reacting to my environment and food, as well as having other symptoms of Hashimoto's (like brain fog, hair loss, fatigue, and anxiety), was overwhelming, to say the least. It took me some time to sort everything out and get to my root causes. My hope is that this article provides you with helpful information, clarity, and next steps in your own journey of discovery.
In this article, you'll discover:
- What histamine is, and what it means to have an intolerance
- What DAO is, and how it relates to histamine
- Testing strategies for histamine intolerance
- The histamine and thyroid connection
- Histamine intolerance treatments
What is Histamine?
Histamine is an important chemical in the immune system that is released by cells during hypersensitivity or inflammatory reactions. In simple terms, when your body is exposed to an allergic compound, histamine increases and turns on inflammation in order to protect the body from that compound. Histamine causes the contraction of smooth muscles and the dilation of blood vessels, which allow immune cells to travel to the site of the perceived attack. In normal amounts in the body, histamine helps with circulation, attention, and digestion, and is also considered a neurotransmitter.
Your body cells make histamine, as do certain bacteria and yeast in your digestive tract. Histamine is also found in some foods.
Histamine is associated with allergic or sensitivity reactions. In the springtime when pollen comes out, many people experience watery eyes, a runny nose, and itchy skin. This is a histamine reaction. You've likely heard of antihistamine medications or supplements designed to dampen this type of reaction.
How Does Histamine Relate to DAO?
DAO, or diamine oxidase, is an enzyme produced by healthy gut cells that breaks down histamine in the small intestine. HNMT (Histamine N-Methyltransferase) is the enzyme responsible for breaking down histamine within the body, but when it comes to histamine intolerance, I am mainly referring to DAO and its role within the digestive system.
The body's preferred state is to have a nice balance between histamine levels and DAO enzymes, in the digestive tract.
What is Histamine Intolerance?
Simply put, histamine intolerance occurs when there are not enough DAO enzymes to balance the levels of histamine in the digestive system.
Unlike a true allergy, histamine intolerance may not be an immediate reaction. Histamine levels build over time, as the body is not able to keep up with DAO production, or histamine levels are too high. Like I mentioned, the body produces histamine, but histamine also enters the body via food. The bacteria on food can produce and release histamine, and other foods may cause the body to release histamine in response.
Symptoms of Histamine Intolerance
Symptoms of histamine intolerance are widespread and may be non-specific, making histamine intolerance difficult to diagnose. Often, histamine intolerance may be mistaken for a food allergy, food sensitivity, mast cell disorder, and other diagnoses.
Individuals with histamine intolerance may experience some of these symptoms listed below, but not others. Bloating may be the most common symptom, along with fullness after a meal, diarrhea, abdominal pain, and constipation. These symptoms may be similar to symptoms of SIBO.
Common Histamine Intolerance Symptoms
- Stomach pain, cramping
- Nausea, vomiting
- Diarrhea, constipation
- Headaches and migraines
- Low blood pressure
- Heart arrhythmia
- Hives, itching, flushing
- Runny nose
- Swelling in the face, mouth or throat
- Asthma
- Fatigue
- Dysmenorrhea (menstrual cramping)
The Histamine and Thyroid Connection
Those with thyroid imbalances, including Hashimoto's, may be more susceptible to histamine intolerance. This may be because histamine intolerance and Hashimoto's thyroiditis can share the same root causes, including:
- Gluten sensitivity
- Leaky gut
- SIBO
- IgE allergies
What's more, in attempts to heal the thyroid, some may inadvertently increase high histamine foods in their diet, discover they have a deficiency in the DAO enzyme, or unknowingly be consuming substances that block DAO. I will cover each of these topics below, in the treatment section.
Diagnosis and Testing
Testing and diagnosis for histamine intolerance is emerging. Currently, many functional and naturopathic doctors test for blood levels of DAO as an indicator of the body's ability to break down histamine. Urine histamine testing is also being developed and implemented as a new, and likely much easier, testing option. However, both of these tests still may not be widely available.
Some may choose a trial of a DAO supplement or a histamine elimination diet to see if symptoms reduce. Both of these options are discussed in more detail below.
Genetic testing may also be helpful. Looking for SNPs (single nucleotide polymorphisms) in the genes that code for the DAO and HNMT enzymes can often provide a piece of the puzzle.
Conventional Treatments
The conventional approach to treating histamine intolerance often looks toward medications such as antihistamines. If you have seasonal allergies, you might already be inclined to reach for antihistamines, because symptoms can be similar. The upside to antihistamines might be some momentary relief. However, they don't address the root cause and, therefore, they're not the most effective solution.
Antihistamines may also decrease DAO production in the body.
The Root Cause Approach
As you know, I love digging deeper and looking at the root cause. I find this to be the most reliable way to promote healing and create long-term health changes. When it comes to treating histamine intolerance, here are some root causes to consider:
1. Remove gluten.
When treating the root cause of Hashimoto's, a gluten-free trial is well warranted because of the connections between gluten-sensitivity and thyroid health. When talking about Hashimoto's and histamine intolerance, we can often see even more of a connection. In those with non-celiac gluten sensitivity, it is possible that gluten is reducing DAO production in the gut, and removing gluten may be a simple root cause solution.
2. Address intestinal permeability (and check for SIBO).
Groundbreaking research done by Fasano and colleagues found that all cases of autoimmunity have some degree of intestinal permeability (commonly referred to as "leaky gut," though if you use that term with a conventionally-trained physician, he/she may look at you like you have three heads!), a genetic predisposition, and a triggering event.
Zonulin is a protein that is released in excess when the gut becomes permeable. This can now be measured — although I don't often test this clinically, as the cut-off range can be misleading in my opinion, and most people who are not in remission will have a leaky gut. However, this test is often super relevant in research studies. A 2018 study showed elevated levels of zonulin and dysbiosis (bacterial imbalances in the gut) in people with histamine intolerance.
So, healing the intestinal permeability not only addresses histamine intolerance, but helps to heal the root cause of Hashimoto's as well.
"Healing the gut" is a term that is widely thrown out into the blogosphere by natural health advocates, and one may think that all is required is eliminating a few foods, and perhaps some bone broth. While these two things can be helpful, I want to be sure to stress that there are multiple causes of intestinal permeability (not just food sensitivities or a "bone broth" deficiency). In my experience, elimination diets can help the symptoms, but don't usually heal most cases of leaky gut. With a few important exceptions (gluten, dairy, and potentially soy), food sensitivities are a symptom, not a cause, of leaky gut.
In my experience, I've seen that people who have chemical sensitivities/multiple allergies, as well as histamine intolerance, often do really well with my liver protocol (or something similar) before diving into a gut support protocol like the one I outlined in Hashimoto's Protocol , with modifications to avoid consuming high histamine (bone broth and fermented veggies, which are typically great for supporting the gut, are both high histamine foods).
Another important root cause of intestinal permeability and digestive symptoms is SIBO, or small intestinal bacterial overgrowth. This generally means that bacteria from the large intestine have migrated up in the small intestine. The bacteria may ferment foods there, and that may cause gas, bloating, and indigestion. SIBO is known to be a potent cause of leaky gut.
Up to 50 percent of people with Hashimoto's may have SIBO, possibly due to low thyroid hormone that slows down movement through the digestive system, among other factors. Hypothyroidism, slowed motility, and SIBO seem to fuel one another, and some practitioners who specialize in SIBO think that hypothyroidism is the trigger for SIBO… while others like yours truly, believe that SIBO triggers hypothyroidism though the autoimmune/leaky gut mechanism. Both scenarios are possible. 🙂
Since certain species of bacteria can be histamine producers, SIBO can exacerbate the amount of histamine in the gut and increase the need for DAO production. What's more, since the gut may be leaky, this histamine has an easier time making it into the body, where it can cause a host of uncomfortable symptoms.
Addressing the microbial imbalances and restoring the integrity of the gut lining, may have a profound impact on one's ability to tolerate histamine again. It may also increase DAO production.
3. Test for IgE allergies and avoid them.
IgE allergies are known as "true allergies" (though I always think this terminology is misleading). They can cause symptoms like wheezing, shortness of breath, and skin reactions. Symptoms are going to be more immediate (minutes) when compared to food sensitivities that are often delayed (hours to days). People with IgE food allergies often have an impaired capacity to break down histamine in the digestive system, so if someone is continually eating a food they are allergic to, it could be the cause of the increased histamine.
The most common IgE food allergens are milk, egg, soy, wheat, peanuts, tree nuts, fish, and shellfish. Other non-food IgE allergens that we commonly see include dust, pollen, animal dander, and certain types of grasses. Environmental allergies will usually cause symptoms such as sneezing and stuffy nose, while food allergies typically present with symptoms such as coughing, shortness of breath, hives, and abdominal pain.
One form of treatment for allergies is an allergy shot. It works as an immunotherapy, wherein a tiny amount of the allergen is delivered through an injection over a period of time, in order to stimulate the immune system to build a tolerance to the allergen, so that it no longer reacts. While allergy shots can be effective for people with environmental allergies, they are less effective for food allergies and are not generally recommended.
An alternative form of allergy treatment, called sublingual immunotherapy (SLIT), involves giving a patient small doses of an allergen under the tongue, to boost tolerance to the substance, and reduce symptoms. This form of allergy therapy is generally considered safe and has several published studies showing its effectiveness for a wide range of allergies. An added benefit is that the patient is able to administer maintenance doses of the prescribed allergen themselves, without returning to the allergist's office for treatments.
4. Address DAO blockers.
Alcohol and tea (green and black tea) may block DAO from doing its job to break down histamine. Avoiding these in one's diet may be a helpful part of improving tolerance to histamine.
Certain medications also release histamine or block DAO. These may include: muscle relaxants, narcotics, pain medications (NSAIDs), antihypertensives, antiarrhythmics, diuretics, drugs that speed up gut motility, antibiotics, histamine (H2) blockers, antidepressants, and others. If you are suffering from symptoms of histamine intolerance, it may be helpful to review medications with your provider and pharmacist.
5. Avoid high histamine foods.
Avoiding high histamine foods may be helpful for reducing symptoms of histamine intolerance while the other root causes are addressed. As the gut heals and other triggers are removed, it is likely that these foods will be able to be introduced again at some point, with better tolerance.
One study showed that a low histamine diet can increase the body's own production of DAO.
Another study showed that either boiling plant foods or insuring maximum freshness of foods, can lower one's histamine reaction. This is because as foods age and ferment, bacteria on the foods can release more histamine. This is one reason that you may not have a reaction to a fresh cooked meal, but you do experience a reaction to the leftovers a couple days later.
The following food lists can provide guidance for a starting point. Consider eliminating the high histamine foods for a period of 30 days, and then begin to slowly reintroduce foods. The process is the same as my elimination diet; however, the food lists are different.
How to Do an Elimination Diet with High Histamine Foods
An elimination diet requires you to remove the most common food sensitivities from your diet for a period of three weeks. It is imperative during this time that you do not "cheat" at all by eating even a small amount of any of the foods that have been removed. Doing so could cause a reaction and interfere with your results.
There are three important steps to the elimination diet:
- Decide which foods you are going to eliminate. If you are looking to identify and heal from histamine intolerance, you will need to avoid all foods that are high in histamine. See the food list below.
- Avoid the foods you are eliminating. This step is crucial! Again, even the smallest amount of a food that you are avoiding could cause a reaction, so it is important that you are vigilant and avoid all traces of the food for three weeks. Check food labels carefully, and be extra careful if you are eating out, as it's difficult to know all of the ingredients used in restaurants. It may be best to avoid eating out during this elimination period, to avoid any cross-contamination that might skew your results.
- Reintroduce the challenged foods. If your symptoms have improved after 30 days, you can start adding the foods back in, one at a time. Paying attention to any reactions you may have to particular foods will help you identify your personal food sensitivities.
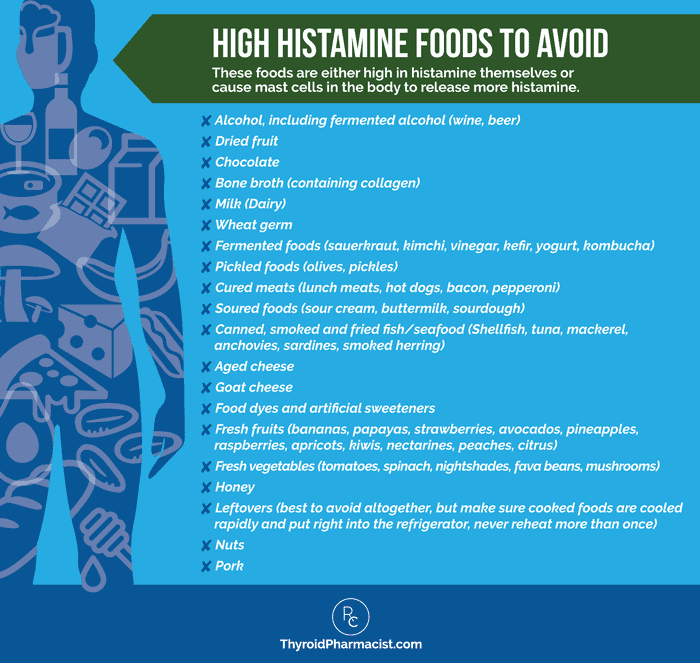
High Histamine Foods to Avoid
These foods are either high in histamine themselves, or cause mast cells in the body to release more histamine:
- Alcohol, including fermented alcohol (wine, beer)
- Dried fruit
- Chocolate
- Bone broth (containing collagen)
- Milk (dairy)
- Wheat germ
- Fermented foods (sauerkraut, kimchi, vinegar, kefir, yogurt, kombucha)
- Pickled foods (olives, pickles)
- Cured meats (lunch meats, hot dogs, bacon, pepperoni)
- Soured foods (sour cream, buttermilk, sourdough)
- Canned, smoked and fried fish/seafood (shellfish, tuna, mackerel, anchovies, sardines, smoked herring)
- Aged cheese
- Goat cheese
- Food dyes and artificial sweeteners
- Fresh fruits (bananas, papayas, strawberries, avocados, pineapples, raspberries, apricots, kiwis, nectarines, peaches, citrus)
- Fresh vegetables (tomatoes, spinach, nightshades, fava beans, mushrooms)
- Honey
- Leftovers (best to avoid altogether, but make sure cooked foods are cooled rapidly and put right into the refrigerator; never reheat more than once)
- Nuts
- Pork
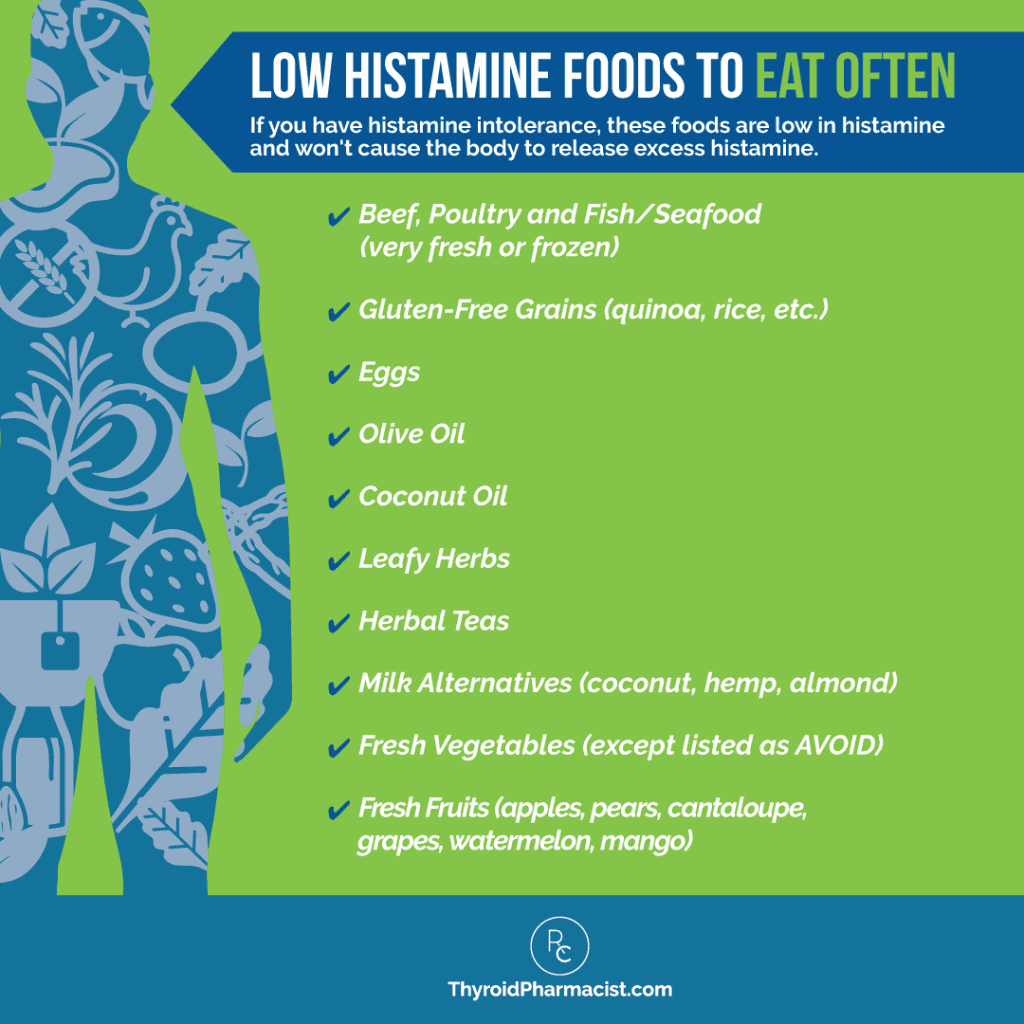
Low Histamine Foods to Eat Often
- Beef, poultry and fish/seafood (very fresh or frozen)
- Gluten free grains (quinoa, rice, etc.)
- Eggs
- Olive oil
- Coconut oil
- Leafy herbs
- Herbal teas
- Milk alternatives (coconut, hemp, almond)
- Fresh vegetables (except those listed as AVOID)
- Fresh fruits (apples, pears, cantaloupe, grapes, watermelon, mango)
6. Include quercetin-rich foods in your diet.
Quercetin is a natural pigment that can be found in many fruits and vegetables. It is high in antioxidants and plays an important role in combating free radicals, as well as reducing inflammation, allergy symptoms, and blood pressure. Animal studies have found that quercetin may block enzymes involved in inflammation, and suppress inflammation-promoting chemicals, such as histamine.
Quercetin-Rich Foods to Eat Often and Combine with High Histamine Foods
- Fresh fruits (apples, plums, cranberries and juice, black currants, capers)
- Fresh vegetables (kale, onions – all varieties, red being the highest, spinach)
- Fresh herbs (tarragon, watercress, chives, coriander, lovage, dill)
- Cocoa powder (raw)
Supplements to Address Histamine Intolerance
In addition to reducing the amount of histamine you consume through foods, there are a few helpful supplements that can help with symptoms of histamine intolerance.
1. DAO – A low histamine diet combined with DAO supplementation can improve one's symptoms and quality of life. For those with migraine headaches, DAO supplementation has been shown to reduce the duration of their migraine attack by 1.4 hours, and another study has shown that people with migraine headaches tend to have low DAO in their blood. DAO may be effective for other symptoms as well, and is often worth a trial. Be sure to work with a practitioner to help you find a DAO supplement that works best for your needs.
2. Vitamin C – Vitamin C can help with symptoms of histamine intolerance, especially when combined with addressing root cause factors. I recommend experimenting with supplementing between 500 and 2000 mg per day, or as recommended by your provider. While high levels of vitamin C are not likely to be harmful, some people may have less bowel tolerance and experience diarrhea at higher doses.
HistaEze by Designs for Health is a combination product that I often recommend. It contains vitamin C, along with electrolytes, nettles, and quercetin, to help with allergies or flares. Stinging nettle and quercetin work together as a natural antihistamine. The dosage is 2 capsules twice per day between meals.
3. Non-Histamine Producing Probiotics – Many probiotics actually produce histamine and may even contribute to histamine intolerance, especially when leaky gut or SIBO are present.
Spore-based probiotics, such as MegasporeBiotic and Saccharomyces Boulardii, tend to be well tolerated by those with histamine intolerance, and may be helpful for gut healing.
For both of these supplements, the recommended dosage is 2 capsules per day, with food.
4. Liver and Gallbladder Support – Liver and Gallbladder Support by Rootcology may be a helpful addition to your supplement plan, especially during times of flares, or when seasonal or environmental allergies are also at play. This supplement contains vitamins A, B6 and B12, along with L-methionine, milk thistle, taurine, inositol, ox bile, artichoke, and beets. It offers support during times of GI distress, and is especially helpful for those who need additional liver and gallbladder support. It is not for those with a history of Addison's, electrolyte imbalance, diuretic use, or steroid medication use.
5. Camel Milk – While not technically a supplement, when camel milk is well tolerated, it has some interesting properties to help heal Hashimoto's and support food sensitivities, including histamine intolerance. There is evidence to suggest it's beneficial for immune system balance, thyroid hormone balance, blood sugar balance, resolving food sensitivities, and reducing nutrient deficiencies.
One of my clients shared: "Both of my daughters' and my own histamine reactions have significantly improved. My 5-yr old was on daily antihistamines because she had stomach pain and itching after every meal. Two weeks drinking camel milk, and I was able to take her off them."
If this food-as-medicine approach resonates with you, and it feels like a good fit, then Desert Farms Camel Milk is a great option!
Next Steps
As with many healing journeys, the journey with histamine intolerance may be multifaceted, and requires patience and persistence. Taking a root cause approach can offer lasting results, so I'm glad you now have some tools to get started with. As I mentioned, I often hear stories of people who are able to tolerate high histamine foods to some degree, after healing the gut and supporting DAO… so change is possible!
Healing Histamine is the website and life's work of Yasmina Ykelenstam, an exceptional, passionate, and beautiful pioneer in histamine intolerance, and also a friend of mine who recently passed away due to breast cancer.
While I only had the pleasure of meeting Yasmina a few times, she had this vibrance about her that made people love her almost immediately after meeting her. She was fierce, fun, dedicated, and brilliant.
Her site has a host of information, resources, and recipes that fit in line with addressing the root causes of histamine intolerance. According to personal communication with Yasmina, she has also found the following supplements extremely helpful:
- NeuroProtek: This supplement was created by the National Institutes of Health, funded Dr. Theoharides (mast cell researcher) at Tufts. It stabilizes mast cells and prevents them from releasing inflammation, while also acting as an antihistamine.
- Mangosteen: This fruit inhibits mast cell histamine release and prostaglandin synthesis, as well as helps with IgE allergies.
- Holy basil: This adaptogenic herb is excellent for stress relief, and is an effective antihistamine and mast cell stabilizer.
Yasmina's website also contains a helpful high histamine food list, as well as information on getting a diagnosis. I know her work will continue helping people for many years to come.
For more information about addressing the root causes of Hashimoto's, I encourage you to pick up a copy of Hashimoto's: The Root Cause . My cookbook Hashimoto's Food Pharmacology contains many histamine diet-friendly recipes that can help you on your journey to healing as well.
Now, I'd like to hear from you! Please share your experience with histamine intolerance and Hashimoto's. What tools, strategies and root cause approaches have served you best?
I wish you all the best on your healing journey!
P.S. Be sure to sign up to my email list to get a free book chapter, recipes, Thyroid Diet start guide, notifications about upcoming events, and my weekly newsletter.
Follow me on Facebook for more news, tips, and the chance to interact with our Hashimoto's community!
References
- Maintz L, Novak N. Histamine and Histamine Intolerance. American Journal of Clinical Nutrition. 2007; 85(5): 1185-96. doi: 10.1093/ajcn/85.5.1185.
- Kovacova-Hanuskova E, Buday T, Gavliakova S, Plevkova J. Histamine, histamine intoxication and intolerance. Allergologia Et Immunopathologia. 2015; 43(5): 498-506. doi: doi: 10.1016/j.aller.2015.05.001.
- Schnedl WJ, Lackner S, Enko D, Schenk M, Holasek SJ, Mangge H. Evaluation of symptoms and symptom combinations in histamine intolerance. Intestinal Research. 2019; Mar 7 (Epub ahead of print). doi: 10.5217/ir.2018.00152.
- Comas-Baste O, Latorre-Moratalla ML, Bernacchia R, Veciana-Nogues MT, Vidal-Carou MC. New approach for the diagnosis of histamine intolerance based on the determination of histamine and methylhistamine in urine. Journal of Pharmaceutical and Biomedical Analysis. 2017; 145: 379-385. doi: 10.1016/j.jpba.2017.06.029.
- Schnedl WJ, Lackner S, Enko D, Schenk M, Mangge H, Holasek SJ. Non-celiac gluten sensitivity: people without celiac disease avoiding gluten – is it due to histamine intolerance. Inflammation Research. 2018; 67(4): 279-284. doi: 10.1007/s00011-017-1117-4.
- Schink M, Konturek PC, Tietz E, Dieterich W, Pinzer TC, Wirtz S, Neurath MF, Zopf Y. Microbial patterns in patients with histamine intolerance. Journal of Physiology and Pharmacology.2018; 69(4). doi: 10.26402/jpp.2018.4.09.
- Lackner S, Malcher V, Enko D, Mangge H, Holasek SJ, Schnedl WJ. Histamine-reduced diet and increase of serum diamin oxidase correlating to diet compliance in histamine intolerance. European Journal of Clinical Nutrition. 2019; 73(1): 102-104. doi: 10.1038/s41430-018-0260-5.
- Sanchez-Perez S, Comas-Baste O, Rabell-Gonzalez J, Veciana-nogues MT. Biogenic Amines in Plant-Origin Foods: Are They Frequently Underestimated in Low-Histamine Diets. Foods. 2018; 7(12). doi: 10.3390/foods7120205.
- Izquierdo-Cassas J, Comas-Baste O, Latorre-Moratalla ML, Lorente-Gascon M, Duelo A, Soler-Singla L, Vidal-Carou MC. Diamine oxidase (DAO) supplement reduces headache in episodic migraine patients with DAO deficiency: A randomized double blind trial. Clinical Nutrition. 2019; 38 (1): 152-158. doi: 10.1016/j.clnu.2018.01.013.
- Izquierdo-Cassas J, Comas-Baste O, Latorre-Moratalla ML, Lorente-Gascon M, Duelo A, Vidal-Carou MC, Soler-Singla L. Low serum diamine oxidase (DAO) activity levels in patients with migraine. Journal of Physiology and Biochemistry.2018; 74(1): 93-99. doi: 10.1007/s13105-017-0571-3.
Vitamin C Dosage For Histamine Intolerance
Source: https://thyroidpharmacist.com/articles/histamine-and-hashimotos/

Tidak ada komentar: